Ambulance and Medical Transport Services - CAM 100105
Description:
Medical transport services involve the use of specially designed and equipped vehicles to transport ill or injured patients. These services may involve ground, air or water transport in both emergency and specialty care transport situations.
Policy:
Emergency Medical Transport
Emergency medical transport services are medically necessary when the following criteria are met:
- The emergency medical transport services must comply with all local, state and federal laws and must have all the appropriate, valid licenses and permits.
- The emergency medical transport must have the necessary patient care equipment and supplies.
- The patient must be transported from the scene of a life-threatening (or perceived to be life threatening by on-site providers) accident or emergency to the nearest hospital or appropriate medical facility for the treatment of the individual’s illness or injury.
Specialty Care Transfer
Medical transport for specialty care is MEDICALLY NECESSARY when the following criteria are met:
- The medical transport services must comply with all local, state and federal laws and must have all the appropriate, valid licenses and permits.
- The medical transport must have the necessary patient care equipment and supplies.
- The patient is currently in an acute care hospital and the specialized services that the patient requires are not available in that facility.
- The destination facility is the nearest provider that has the specialized services the patient requires.
Unless the below criteria for Air Transport are met, ground transport will be considered Medically Necessary for emergency medical transport and specialty care transfer that meet the above criteria.
Air or Water Transport
Air or water transport services may be MEDICALLY NECESSARY for emergency medical transport or specialty care transfer when the following criteria are met:
- The individual’s location is such that accessibility is only feasible by air or water transportation.
- The individual’s condition is such that the time needed to transport by ground poses a threat to the individual’s survival or seriously endangers the individual’s health. This may include, but is not limited to, the following:
- Intracranial bleeding; or
- Cardiogenic shock; or
- Major burns requiring immediate treatment in a Burn Center; or
- Conditions requiring immediate treatment in a Hyperbaric Oxygen Unit; or
- Multiple severe injuries; or
- Transplants; or
- Limb-threatening trauma; or
- High risk pregnancy; or
- Ischemic Stroke; or
- Acute myocardial infarction; if this would enable the individual to receive a more timely medically necessary intervention (such as percutaneous transluminal coronary angioplasty [PTCA].
Air transportation may be appropriate in certain clinical situations if the time between identification of the need for transportation (e.g. Dispatch Time) until arrival at the intended destination for ground transport would result in significant time delay (e.g. 30 minutes to 1 hour) longer than air transport. Transportation time discrepancy evaluation will be determined on an individual case-by-case basis.
Non-Emergency Medical Transfer
Nonemergency transfer will be considered MEDICALLY NECESSARY to transfer from a prior authorized higher level of care admission to a lower level of care admission (e.g., from a prior authorized inpatient hospital admission to a prior authorized skilled nursing facility) when the member's condition makes other forms of transportation infeasible (e.g., mechanical ventilation, traction). This transportation may require prior authorization according to the member’s plan.
Policy Guidelines:
Emergency Medical Transport services or Specialty Care Medical Transport services are considered NOT MEDICALLY NECESSARY if the patient is not transported to a health care facility .
Emergency Medical Transport services are considered NOT MEDICALLY NECESSARY if the patient is legally pronounced dead before the emergency medical transport was dispatched .
Emergency Medical Transport services may be considered MEDICALLY NECESSARY if the patient is legally pronounced dead after the emergency medical transport was dispatched but before pickup or en route to the hospital.
Professional Societies/Organizations
The American College of Emergency Physicians and National Association of EMS Physicians (NAEMSP) published guidelines for the utilization of air medical transport including clinical situations for scene triage, air transport (also known as primary air transport), and inter- facility transfers. This position statement has been endorsed by the Air Medical Physician Association (AMPA) (Thomson, et al., 2003).
The following lists of indications are not all-inclusive:
Scene triage for air transport to Health Care Facility:
Trauma
- General and mechanism considerations:
- Trauma Score less than 12, (Glasgow Coma Scale, Systolic Blood, Pressure Respiratory)
- Unstable vital signs (e.g., hypotension or tachypnea)
- Significant trauma in patients less than 12 years old, greater than 55 years old, or pregnant patients
- Multisystem injuries (e.g., long-bone fractures in different extremities; injury to more than two body regions)
- Ejection from vehicle
- Pedestrian or cyclist struck by motor vehicle
- Death in same passenger compartment of the vehicle as patient
- Ground provider perception of significant damage to patient’s vehicle’s passenger compartment
- Penetrating trauma to the abdomen, pelvis, chest, neck, or head
- Crush injury to the abdomen, chest, or head
- Fall from significant height
- Neurologic considerations: Glasgow Coma Scale score less than 10 †
- Deteriorating mental status
- Skull fracture
- Neurologic presentation suggestive of spinal cord injury
- Thoracic considerations:
- Major chest wall injury (e.g., flail chest)
- Pneumothorax/hemothorax
- Suspected cardiac injury
- Abdominal/pelvic considerations:
- Significant abdominal pain after blunt trauma
- Presence of a “seatbelt” sign or other abdominal wall contusion
- Obvious rib fracture below the nipple line
- Major pelvic fracture (e.g., unstable pelvic ring disruption, open pelvic fracture, or pelvic fracture with hypotension)
- Orthopedic/extremity considerations:
- Partial or total amputation of a limb (exclusive of digits)
- Finger/thumb amputation when emergent surgical evaluation (i.e., for replantation consideration) is indicated and rapid surface transport is not available
- Fracture or dislocation with vascular compromise
- Extremity ischemia
- Open long-bone fractures
- Two or more long-bone fractures
- Major burns:
- Greater than 20% body surface area
- Involvement of face, head, hands, feet, or genitalia
- Inhalational injury
- Electrical or chemical burns
- Burns with associated injuries
- Patients with Drowning injuries
† The Glascow Coma Scale can be accessed at: https://www.cdc.gov/masstrauma/resources/gcs.pdf
Interfacility Transfers:
- Trauma
- Depending on local hospital capabilities, the Indications listed above under “scene” guidelines may be sufficient indication for air transport; or
- After initial evaluation reveals injuries or potential injuries requiring further evaluation and management beyond the capabilities of the referring hospital.
- Cardiac
- Acute coronary syndromes with time-critical need for urgent interventional therapy unavailable at the referring center (e.g., cardiac catheterization, intra-aortic balloon pump placement, emergent cardiac surgery)
- Cardiogenic shock
- Cardiac tamponade
- Mechanical cardiac disease (e.g., acute cardiac rupture, decompensating valvular heart disease)
- Critically ill medical or surgical patients
- Pre-transport cardiac/respiratory arrest
- Requirement for continuous intravenous vasoactive medications or mechanical ventricular assist to maintain stable cardiac output
- Risk for airway deterioration (e.g., angioedema, epiglottitis)
- Acute pulmonary failure and/or requirement for sophisticated pulmonary intensive care (e.g., inverse-ratio ventilation) during transport
- Severe poisoning or overdose requiring specialized toxicology services
- Urgent need for hyperbaric oxygen therapy (e.g., vascular gas embolism, necrotizing infectious process, carbon monoxide toxicity)
- Requirement for emergent dialysis
- Gastrointestinal hemorrhages with hemodynamic compromise
- Surgical emergencies such as fasciitis, aortic dissection or aneurysm or extremity ischemia
- Pediatric patients for whom referring facilities cannot provide required evaluation and/or therapy
- Obstetric
- Reasonable expectation that delivery of infant(s) may require obstetric or neonatal care beyond the capabilities of the referring hospital
- Active premature labor when estimated gestational age is <34 weeks or estimated fetal weight <2,000 grams
- Severe pre-eclampsia or eclampsia
- Third-trimester hemorrhage
- Fetal hydrops
- Maternal medical conditions (e.g., heart disease, drug overdose, metabolic disturbances) exist that may cause premature birth
- Severe predicted fetal heart disease
- Acute abdominal emergencies when estimated gestational age is <34 weeks or estimated fetal weight <2,000 grams
- Neurological
- Central nervous system hemorrhage
- Spinal cord compression by mass lesion
- Evolving ischemic stroke (i.e., potential candidate for lytic therapy)
- Status epilepticus
- Neonatal
- Gestational age <30 weeks, body weight <2,000 grams or complicated neonatal course (e.g., perinatal cardiac/respiratory arrest, hemo-dynamic instability, sepsis, meningitis, metabolic derangement, temperature instability)
- Requirement for supplemental oxygen exceeding 60%, continuous positive airway pressure (CPAP), or mechanical ventilation
- Extra pulmonary air leak, interstitial emphysema, or pneumothorax
- Medical emergencies such as seizure activity, congestive heart failure, or disseminated intravascular coagulation
- Surgical emergencies such as diaphragmatic hernia, necrotizing enterocolitis, abdominal wall defects, intussusception, suspected volvulus, or congenital heart defects
- Transplant
- Patient has met criteria for brain death and air transport is necessary for organ salvage
- Organ and/or organ recipient requires air transport to the transplant center in order to maintain viability of time-critical transplant
Conceptual Model of the relationship of GEMS and AEMS time in transit from patient loading (“Time 0/Distance 0”) to emergency department bed arrival. (based on authors' consensus)
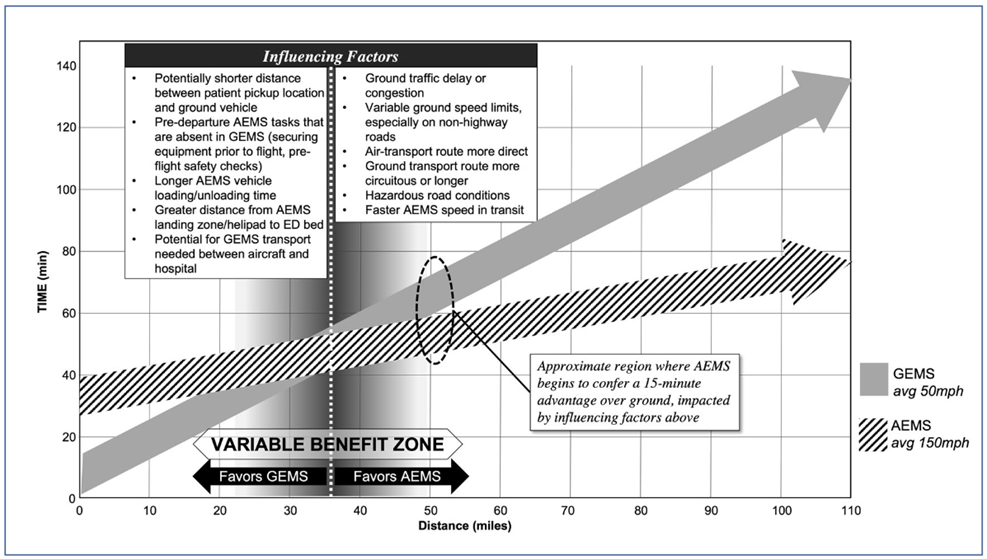
Source: John W. Lyng , Sabina Braithwaite , Heidi Abraham , Christine M. Brent , David A. Meurer , Alexander Torres , Peter V. Bui , Douglas J. Floccare , Andrew N. Hogan , Justin Fairless & Ashley Larrimore (2021) Appropriate Air Medical Services Utilization and Recommendations for Integration of Air Medical Services Resources into the EMS System of Care: A Joint Position Statement and Resource Document of NAEMSP, ACEP, and AMPA, Prehospital Emergency Care, 25:6, 854-873, DOI: 10.1080/10903127.2021.1967534
Coding Section
| Codes | Number | Description |
| CPT | No Code | |
| ICD-9 Procedure | No Code | |
| ICD-9 Diagnosis | No Code | |
| HCPCS | A0429 | Ambulance service, basic life support, emergency transport |
| A0427 | Ambulance service, advanced life support, emergency transport, level 1 | |
| A0433 | Advanced life support, level 2 | |
| A0430-A0431; A0435-A0436 | Ambulance service, conventional air services, transport, one way – code series | |
| A0080-A0210 | Non-emergency transportation (code range) | |
| A0225 | Ambulance service, neonatal transport, base rate, emergency transport, one way | |
| A0380 | BLS mileage (per mile) | |
| A0382-A0384 | BLS disposable supplies (code range) | |
| A0390 | ALS mileage (per mile) | |
| A0392-A0398 | ALS disposable supplies (code range) | |
| A0420 | Ambulance waiting time | |
| A0422 | Ambulance oxygen and oxygen supplies, life-sustaining situation | |
| A0424 | Extra ambulance attendant | |
| A0425 | Ground mileage, per statute mile | |
| A0426 | Ambulance service, advanced life support, non-emergency transport, level 1 (ALS 1) | |
| A0428 | Ambulance service, basic life support, non-emergency transport, (BLS) | |
| A0888 | Non-covered ambulance mileage, per mile (e.g., for miles traveled beyond closest appropriate facility) | |
| A0999 | Unlisted ambulance service | |
| Type of Service | Medical | |
| Place of Service |
Inpatient/Home/Physician's Office |
Procedure and diagnosis codes on Medical Policy documents are included only as a general reference tool for each policy. They may not be all-inclusive.
This medical policy was developed through consideration of peer-reviewed medical literature generally recognized by the relevant medical community, U.S. FDA approval status, nationally accepted standards of medical practice and accepted standards of medical practice in this community, and other nonaffiliated technology evaluation centers, reference to federal regulations, other plan medical policies and accredited national guidelines.
"Current Procedural Terminology © American Medical Association. All Rights Reserved"
History From 2014 Forward
| 09/01/2025 | Annual review, no change to policy intent. |
| 06/04/2025 | Updating entire policy to separate ground and air/water transport. Adding indications for scene triage for air and interfacility transport. |
| 09/03/2024 | Annual review, No change to policy intent. |
| 09/01/2023 | Annual review, No change to policy intent. |
| 09/06/2022 | Annual review, no change to policy intent. |
| 09/07/2021 |
Annual review, no change to policy intent |
| 09/16/2020 |
Annual review, no change to policy intent. |
| 01/07/2020 |
Adding Codes A0426 and A0428 to coding section. No other changes made |
| 12/27/2019 |
Correcting typo. |
| 12/13/2019 |
Interim review to add language related to nonemergency transport. This transport, when preauthorized, will be available effective 01/01/2020. |
| 09/04/2019 |
Annual review, no change to policy intent. |
| 09/10/2018 |
Annual review, no change to policy intent. |
| 09/21/2017 |
Annual review, no change to policy intent. |
| 09/19/2016 |
Annual review, no change to policy intent. |
| 09/14/2015 |
Annual review, no change to policy intent. Added coding. |
| 09/07/2014 |
Annual review, no changes made. |